
Is the goal of gene therapy for cancer to fix the mutation itself?

- Related Topics:
- Cancer,
- Gene therapy,
- CRISPR
An aspiring scientist from San Diego asks:
"Two questions: Is the goal of gene therapy for cancer to fix the mutation itself? Could gene editing be used to treat cancers?"
Gene therapy and gene editing are two types of new therapies that scientists are developing. They may offer hope in the future for patients with currently untreatable cancers.
Gene therapy is a technique that scientists have been investigating for decades. There are a few different methods, but often the goal is to deliver a new gene to a patient. Typically this means the patient will get extra, new DNA to treat a specific genetic condition.
Gene editing is a specific, new type of gene therapy. The goal of this type of treatment is usually to "edit" the patient's own genetic code to fix the underlying problem.
Right now, there are only a handful of gene therapies in the world with FDA approval. Gene therapy is not yet common because it is still being refined and investigated. “Fixing” a mutation is not an easy task!
Cancer is Driven by Genetic Mutations
The cells in our body have checks and balances to make sure that everything is in order. Mutations occur when certain genes are damaged. In cancer, this means that cells grow uncontrollably.
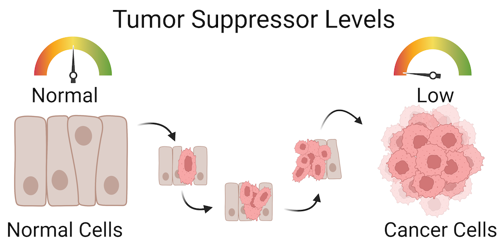
Our cells have a lot of ways to control their growth. For example, there are specific genes that prevent normal cells from dividing uncontrollably into tumors. For that reason, these types of genes are called tumor suppressor genes. But if these genes become damaged, the cells might start dividing too fast and become cancerous.
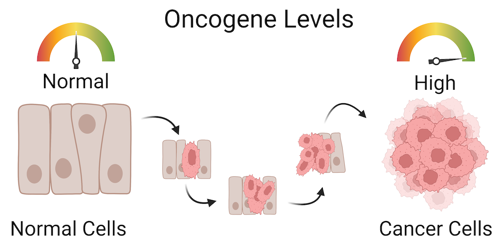
Other types of genes help drive cells through normal cell division and growth cycles. But if these genes become mutated and overactive, the cells will start dividing at a much faster rate. These types of genes are called oncogenes.
Scientists are currently investigating methods to “fix” these two types of cancer mutations.
Innovations in Gene Therapy
Gene therapy is a method used to potentially fix damaged genes. Gene therapy could be used to treat a variety of diseases but cancer treatment is a common goal. There are a few ways that this could be done.
For example, people often have two copies of tumor suppressor genes. When both of these are damaged, tumors can form. By adding an extra, functional copy into the cells, we could prevent uncontrolled division of tumor cells.
That’s exactly what a medication called Gendicine does. Gendicine is injected directly into tumors to express extra copies of the tumor suppressor gene P53. Gendicine was the first gene therapy product to gain regulatory approval, but it is currently still only approved for usage in China.
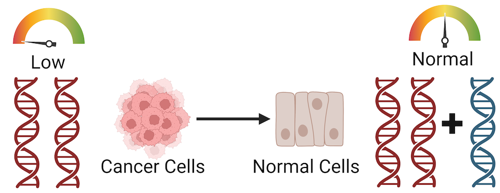
Or if an oncogene is damaged and becomes overactive, adding a copy of a gene that suppresses it could reduce cell division. For example, if someone has an overactive version of the KRAS oncogene, adding an extra copy of a gene that keeps it in check (e.g. PUMA) might help. Gene therapies for the KRAS mutation are still in the early stages of investigation.
While these are the two most common gene therapy approaches for treating cancer, scientists are developing many other strategies as well. For example, CAR T-cell therapy modifies immune cells, which cause the body’s immune system to specifically attack cancer cells.
But right now, gene therapies are still far from being accessible to the general public. There are only a few gene therapies in the entire world with FDA approval, and doctors may only suggest the usage of these therapies in rare situations.
Gene Editing for Treating Cancer
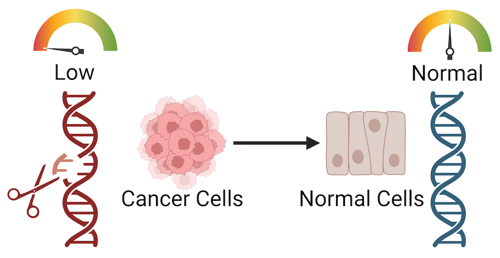
Gene editing is a specific type of gene therapy. Typically the goal of this kind of therapy is to change to the patient’s own DNA to fix cancer mutations. Usually this is done with a gene-editing tool called CRISPR.
CRISPR acts like a pair of scissors to genes. CRISPR consists of a sequence (guide RNA) which tells an enzyme (CAS) where to cut DNA. A new section of DNA can be added at the cut site. In the context of cancer, perhaps the damaged gene is removed and replaced with a functional version. Or maybe small edits are made to the gene sequence so that it works normally again.
CRISPR based gene editing treatments are still in development, and they’re not widely available. CRISPR has only been used for human gene editing during a handful of clinical trials, but even these studies are rare and strictly regulated. The ethics of using CRISPR on humans is a hotly debated topic, and the development of gene editing treatment is still in early stages.
Is Gene Therapy Safe and Effective?
Since gene therapies are so new, it is hard to tell how safe or effective they are compared to other treatments. Most gene therapies are still in development or clinical trials. Only a few have received FDA approval, which happens when the FDA reviews the clinical trial results and agrees that the benefits outweigh any risks. There are many, many potential new therapies being studied now, but it’s a slow process.
There are a variety of side effects that these kinds of therapies could have. For example, short term side effects may occur due to the delivery of a virus into the patient’s body. The patient may experience fevers, chills, nausea, headaches, etc.
Long term side effects include the possibility that the delivered genes end up in healthy cells instead of cancerous ones. These healthy cells could in turn develop another disease or even another kind of cancer. In addition, scientists are worried about the effects of gene therapy on reproductive cells (sperms and eggs). Genetic changes in sperm or eggs could be passed down to future generations.
It also could be hard to treat some cancers with gene therapy. Many gene therapies try to fix one or two specific mutations, but cancer is frequently driven by many different mutations. There are times where fixing one or two mutations within a patient may not be sufficient to treat a rapidly growing tumor.
Gene editing and gene therapy are two exciting methods currently being investigated and trialed as a way to treat cancers. Although these therapies may become the next generation of cancer treatments, there are many safety issues to consider before they become widely available to patients.
Read More:
-
WebMD: Immune cell gene therapy
-
Utah Genetics: Gene therapy approaches
-
Cancer.gov: CRISPR for gene editing

Author: Daiyao Zhang
When this answer was published in 2023, Daiyao was a PhD candidate in the Department of Chemical Engineering, studying the effects of matrix stiffness on pancreatic cancer chemoresistance in Sarah Heilshorn’s laboratory. Daiyao wrote this answer while participating in the Stanford at The Tech program.
 Skip Navigation
Skip Navigation
